Prostate cancer
Male, 61 years, adenocarcinoma, Gleason score 6 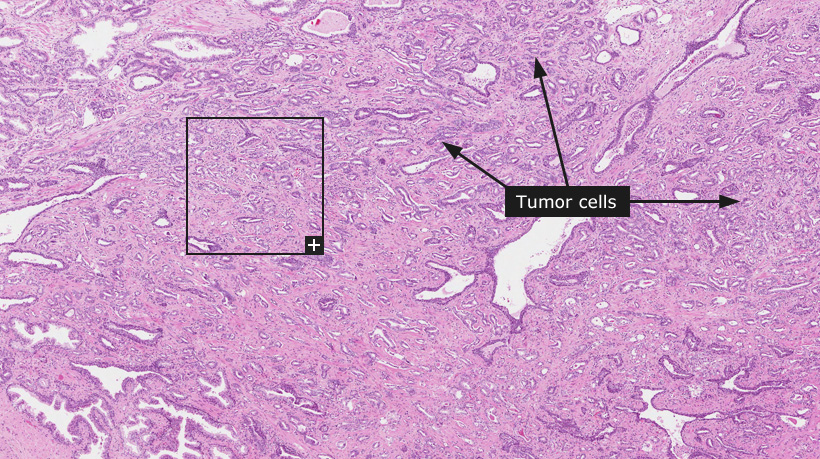
Prostate cancer
Prostate cancer is predominantly a tumor of elderly men and is one of the most common forms of cancer in men in Europe and USA. The rate of tumor growth varies from slow to moderately rapid, and certain patients may have prolonged survival even after the cancer has metastasized to distant sites such as bone. Since the median age at diagnosis is high, most patients - especially those with localized tumors - may die of other illnesses without ever having suffered significant disability from the cancer. Prostate cancer is often stimulated by hormones (androgens) and anti-hormonal therapies can be effective to limit and slow down tumor growth. Radical prostatectomy can also be an option for treating localized prostate cancer. Both normal prostatic glands and prostate cancer cells express PSA (KLK3) and detection of elevated levels of PSA in the blood can indicate the growth of a prostate cancer.
Prostate carcinomas are classified using the Gleason grade (Modified Gleason Grading System). The Gleason grade is a system of characterizing prostate cancer tissue based on the microscopical pattern of growth. The Gleason grade ranges from 1 to 5. Grade 1 is not used in clinical practice as it is impossible to distinguish grade 1 from adenosis and it is considered to lack malignant potential. Gleason grades corresponding to the two dominating growth patterns in a prostate cancer are combined to provide the Gleason score and consequently, Gleason scores range from 4 (2+2) to 10 (5+5). The Gleason score is correlated to the risk of tumor spread. A low Gleason score reflects a more well differentiated tumor while a high Gleason score corresponds to more poorly differentiated tumors. A tumor with Gleason score of 4 is least likely, and tumor with score of 10 is most likely to spread beyond the prostate.
Grade 1 tumors are small, uniform, well-differentiated, closely packed, and consist of glands in essentially circumscribed masses. In Grade 2 there is a moderate variation in size and shape of glands and more atypia in individual cells. A cribriform pattern may be present - still essentially circumscribed - but more loosely arranged. Grade 3 tumors show marked irregularity in size and shape of glands, with tiny glands/individual cells invading into the stroma. Solid cords and masses (papillary or cribriform), with easily identifiable glandular differentiation, vary in size and may be quite large, but the essential feature is a smooth and usually rounded edge around all the circumscribed masses of tumor. In Grade 4, tumor cells grow in a diffuse pattern and may show gland formation, however, glands are not single and separate, but coalesce and branch. Grade 5 tumors are very poorly differentiated, usually presenting solid masses or diffuse growth with little or no differentiation into glands or with a few tiny glands or signet ring cells.
Immunohistochemistry using antibodies towards PSA can be used to distiguish prostate cancer from other forms of cancer. Immunohistochemistry is also important to delineate the two cell types in benign prostatic ducts and acini. The superficial layer is the secretory epithelium, beneath which there is a layer of continuous basal cells in normal glands. Sparse interspersed endocrine-paracrine cells are also present. The basal cells are useful for histologic diagnosis as their presence confirms that the acinus is benign. Their identification is aided by immunohistochemistry stains for p63 and high-molecular weight keratins. Malignant prostatic acini do not display basal cells and are identified using other immunohistochemistry markers such as antibodies towards AMACR/P504S.
Normal tissue: Prostate
|