Cervix, uterine
Cervix, uterine
The uterine cervix accounts for a third to half the length of the uterus and measures 2.5-3 cm in length and 2.0-2.5 cm in diameter in the adult. The vaginal portion of the cervix (portio or exocervix) is surrounded by a reflection of the vaginal wall termed the fornix. The cervix is composed of fibrous, muscular and elastic tissue and is lined by columnar and squamous epithelium. Fibrous tissue is the predominant component. Smooth muscle comprises approximately half the supporting tissue at the region of the isthmus and is almost completely absent in the portio.
Histologically, the mature, non-keratinized stratified squamous epithelium of the exocervix resembles the vaginal epithelium but usually lacks the rete pegs seen in the vagina. Three zones can be identified: the germinal cell layer comprising the parabasal and basal cells, which are oval with scant cytoplasm and perpendicular to the basement membrane. Proliferation is limited to this zone. The maturation occurs in the intermediate or midzone also referred to as the stratum spinosum. Maturation is manifested by an increase in cytoplasmic volume with the accumulation of glycogen, which is responsible for the clear, vacuolated appearance of cells in the upper layers of the epithelium. The superficial zone contains terminally differentiated cells that eventually exfoliate. These cells are flat, have an abundant, eosinophilic cytoplasm and pyknotic nuclei.
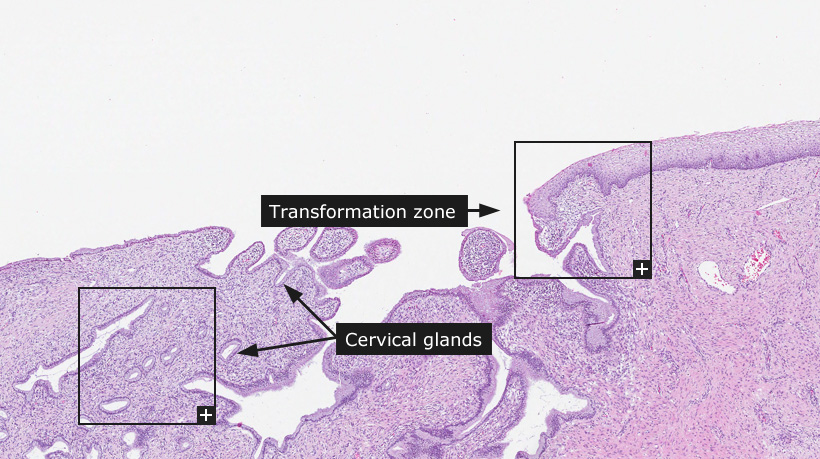
The mucosa of the endocervical canal is composed of a single layer of mucin-secreting, columnar epithelium that lines both the surface and the underlying glandular structures. These "cervical glands" have been shown by three-dimensional studies to be not "true" glands but deep, cleft-like infoldings of the surface epithelium into the underlying stroma. In cross section, the complex infoldings appear as isolated glands. The columnar cells have basal round or oval nuclei and finely granular cytoplasm containing abundant mucin. Mitotic activity is not observed in endocervical cells under normal circumstances.
The "original" squamocolumnar junction and the "new" squamocolumnar junction bound the transformation zone. The "original" squamocolumnar junction is present at birth and normally resides on the exocervix. At about the age of 1 year, the cervix elongates and the squamocolumnar junction migrates towards the external exocervical opening. At the time of menarche and during pregnancy, both the uterus and cervix enlarge. Cervical enlargement is accompanied by a change in cervical shape which results in rolling outwards of the endocervical columnar epithelium onto the portio (exocervix). Over time, the columnar epithelium is replaced by metaplastic squamous epithelium. The newly formed squamocolumnar junction is termed the "new" squamocolumnar junction. Therefore, for most women in the reproductive period, the transformation zone is located on the exposed portion of the cervix. As virtually all squamous cancers, including precancerous lesions (dysplasia), develop at the transformation zone, the vast majority of cervical neoplasias are accessible for diagnosis by punch biopsy.
Cancer: Cervical cancer
|